Healing and Miracles
January 06, 2021The post-transplant chapter of my story has been composed of good days and bad days. A good day is simply a pain-free, nausea-free, having-a-fair-appetite, able-to-shower day, while a bad day is the opposite of that, coupled with tears.
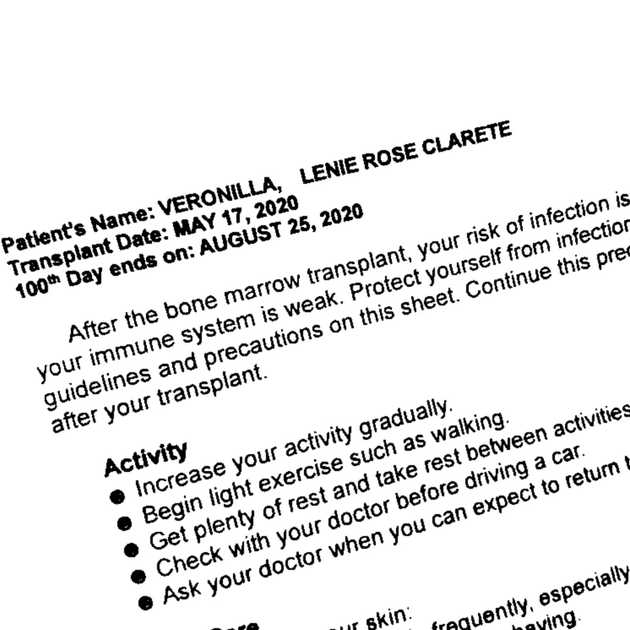
Transplant on May 17 was considered as Day 0 or the day of rebirth. I was discharged from the hospital on Day 24 and I was given a booklet for post-transplant discharge instructions. Guidelines and precautions on activity, nutrition, and more were printed, and a space was provided where I must write my daily weight, vital signs, fluid intake and output, and other notes such as bowel movement. I may be out of the hospital, but it felt like I took the hospital home with me.
Moreover, the home medications were quite overwhelming. For graft-versus-host disease, I was prescribed prograf, cellcept, and prednisone. These are immunosuppressants. To prevent infection, I was prescribed voriconazole (antifungal), valacyclovir (antiviral), and cotrimoxazole (antibacterial). My risk for infection is greater because my immune system is weak. To prevent acidity, I was prescribed with omeprazole. I also have to take magnesium oxide for chronic hypomagnesemia, and ivabradine (anti-angina) and apixaban (anticoagulant) for chronic deep vein thrombosis (blood clot).
Graft-versus-host disease (GvHD) is a potentially serious complication of allogeneic stem cell transplantation and reduced-intensity allogeneic stem cell transplantation. During allogeneic stem cell transplantation, a patient receives stem cells from a donor or donated umbilical cord blood. GVHD occurs when the donor’s T cells (the graft) view the patient’s healthy cells (the host) as foreign, and attack and damage them. Graft-versus-host disease can be mild, moderate, or severe. In some cases, it can be life-threatening. (Leukemia and Lymphoma Society)
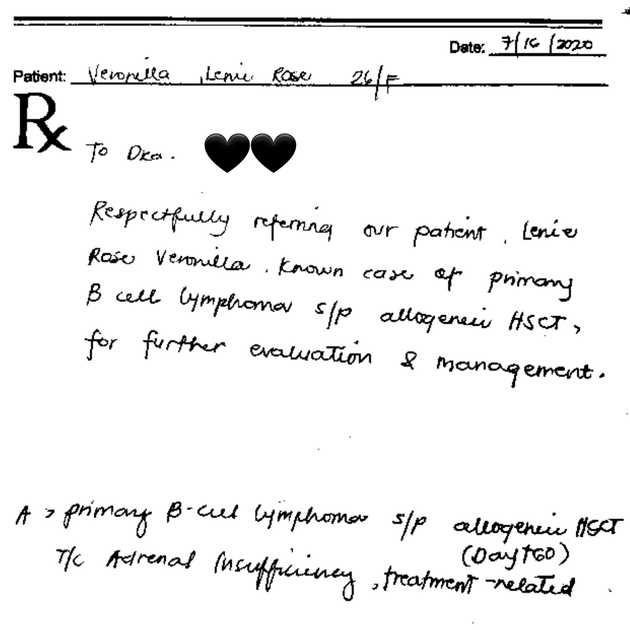
On Day 32, I started having rashes on my neck down to my underarms and on my back. It was GvHD of the skin, so prednisone was increased to 20 mg daily. After a week, my skin improved, and I began tapering down the prednisone. During this period, I was already consistently fatigued that I had to use a wheelchair for my weekly hospital visit and on my bad days, my mother had to feed me. Brushing my teeth also took great effort. But when prednisone was down to 10 mg daily, I experienced extreme fatigue and headache. My oncologist suspected adrenal insufficiency, so I had my cortisol, a steroid hormone, checked.
My cortisol assay was at 3.7 when it was supposed to be at 4.30-22.40. Hence, on Day 60, I was referred to an endocrinologist, who requested for tests to determine my lipid profile, blood sugar, and some thyroid and reproductive hormones.
The test results revealed adrenal insufficiency, hyperlipidemia, and menopause.
For adrenal insufficiency, prednisone was increased back to 20 mg daily, and if I were to start tapering down again, I must taper very slowly. For hyperlipidemia, I was prescribed with fenofibrate; notably, my triglycerides subsequently decreased to 116 from 523 (normal is below 150). For menopause, the doctor could prescribe hormone pills to manage symptoms, but I was hesitant because I am taking anticoagulant medication, which I believe is a contraindiction. I also asked if I had permanent or temporary menopause. The doctor replied that I have to see a reproductive endocrinologist for further evaluation and fertility options.
In addition, the doctor instructed me to start monitoring my blood sugar levels at home because prednisone may cause a spike. The doctor also prescribed calcium and vitamin D because prednisone may cause osteoporosis.
Encountering complications and setbacks in my healing and recovery motivated me more to acknowledge and celebrate small wins, like being able to travel without a wheelchair for my weekly hospital visit by the end of July.
On Day 76, prednisone was further increased to 40 mg daily because I was once again experiencing GvHD of the skin. This time, rashes were all over my limbs. My only consolation was increased energy from the high-dose steroid because the other side effects of prednisone were simply unpleasant. From Day 88 onwards, when my skin was improving, I started tapering down the prednisone by 10 to 5 mg.
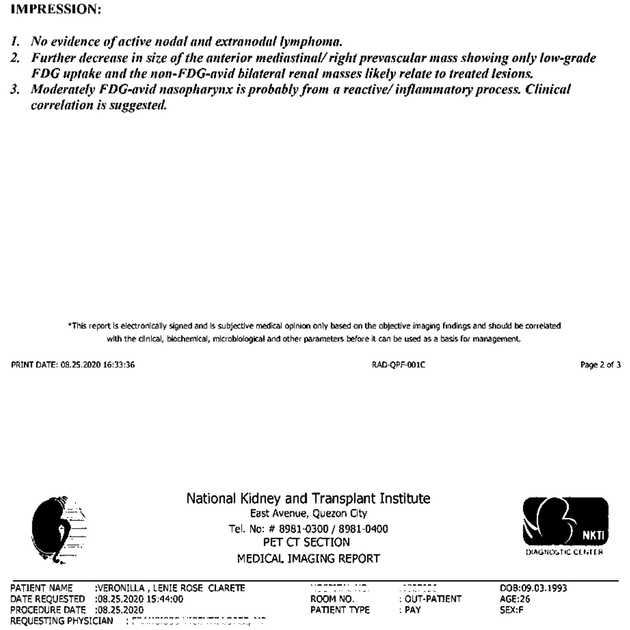
On August 25, I celebrated reaching Day 100. On the same day, I had my post-transplant PET/CT. And praise Jesus, I am still in remission! It was an early birthday present because on September 3, I turned 27.
By mid-September, I was on prednisone 15 mg daily, but on Day 128, my SGPT, a liver enzyme, spiked at 537 (normal is 15-59). Hence, prednisone was increased back to 20 mg daily. But the following week, my SGPT further spiked at 1180! It was GvHD of the liver. So, prednisone was again at 40 mg daily, and I was prescribed Godex. Although my SGPT was extremely high, surprisingly, I had this quiet confidence that I will be alright.
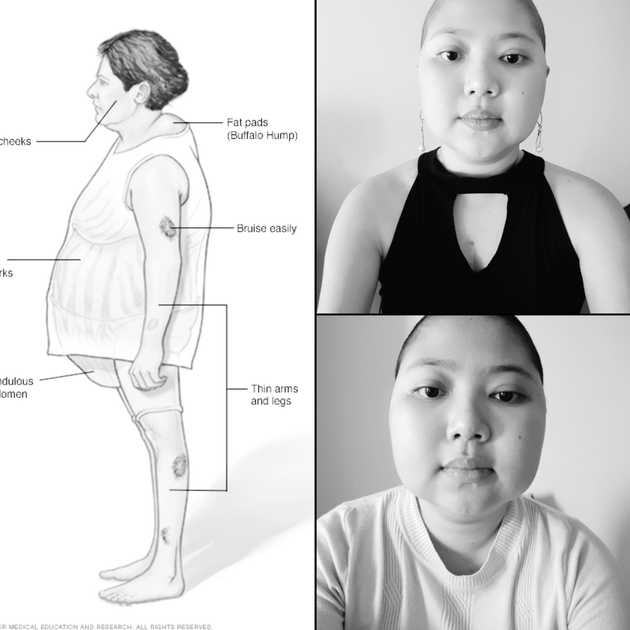
Prednisone is a two-edged sword: it is treating GvHD, but it also has nasty side effects. I felt hungry all the time! I woke before the sun rose! But insomnia and the occasional muscle pains were tolerable. My self-image, on the other hand, was twisted. Honestly, I was more disappointed on being on high-dose steroid than having GvHD because I did not like how I looked and felt. I had a cushingoid appearance: facial puffiness, or moon face, and fatty hump between the shoulders, or buffalo hump. I was also gaining weight, around 10 kg, mostly distributed on my midsection; probably because of water retention and increased appetite.
I was earnestly praying to God to resolve the GvHD because the faster my SGPT decreased, the sooner I will be able to taper down the prednisone and maybe the sooner I will look and feel better. Embarrassed, I realized how shallow my motivation was shallow and changed my prayer. Though I still ask God that I will be able to taper off prednisone successfully and not encounter adrenal insufficiency again, I foremost ask Him to increase my patience and gratitude, and to transform my self-image positively.
From October to November, my SGPT was gradually decreasing. Subsequently, I started tapering down the prednisone. By December, I was on prednisone 10 mg daily and started very slowly tapering down by 2.5 mg on selected days. My hospital visits were also changed from weekly to biweekly. Almost all my blood counts and chemistry levels were normal. On paper, I was doing good, but in person, I was feeling otherwise! I had significantly decreased energy, low mood, and poor appetite. I frequently had nausea and headaches. I also noticed tremors. Maybe I was experiencing a little steroid withdrawal. It was challenging to identify which medication is really causing which side effect or to identify symptoms as consequences of the transplantation and previous therapies. As long as my symptoms were nothing serious, I endured.
On Day 214, after more than two months of elevated SGPT, it was finally normal at 48. Thank You, Jesus!
However, I started having rashes again. This time, I was referred to a dermatologist, who said that the rashes looked like telangiectases or spider veins, and that if it was skin GvHD, it is Grade 1 and requires no treatment, although the doctor prescribed Hirudoid cream for relief.
As of this writing, I am on Day 234. I am due for my biweekly hospital visit tomorrow and another PET/CT on February or March. I pray that I will still be in remission and that the result of the scan will be favorable for a ureteral stent removal.
Just as I declared in the beginning of 2020, I truly received healing and miracles. But it was a bittersweet victory. 2020 was generally a bad year because of COVID-19. Many lives were lost, and not only because of the virus itself. My friends, whose cancer treatment were significantly affected by the pandemic, passed away. There was survivor’s guilt. But entering 2021, I still hope for more healing and miracles. I hope to embody a character and a perspective that are pleasing to God. And I hope that whatever lies ahead, I will be able to always respond in faith.